The Aspirin Debate: Does Preventive Use Truly Reduce Mortality Risks?
Aspirin and Its Controversial Role in Preventive Medicine
Aspirin has long been considered a cornerstone of preventive medicine, with recommendations for its use in reducing the risk of cardiovascular disease (CVD) spanning several decades. However, its overall impact on mortality has remained uncertain. According to a recent study, the use of aspirin for primary prevention does not consistently improve health outcomes. Among U.S. adults aged 40 and older, low-dose aspirin (≤100 mg/day) showed no significant reduction in mortality from any cause, while high-dose aspirin (>100 mg/day) was linked to an alarming increase in deaths related to CVD.
This contrast raises important questions about the widespread use of aspirin as a preventive measure and whether its potential risks outweigh its benefits.
High-Dose Aspirin: A Potential Risk for Cardiovascular Mortality
Research shows concerning findings regarding high-dose aspirin use. Participants who took more than 100 mg per day were found to have a significantly increased risk of cardiovascular disease (CVD) mortality, with a hazard ratio of 1.63 (95% confidence interval: 1.11–2.41). This risk was particularly notable in individuals aged 60 and older, indicating that high-dose aspirin could pose greater cardiovascular risks for vulnerable populations.
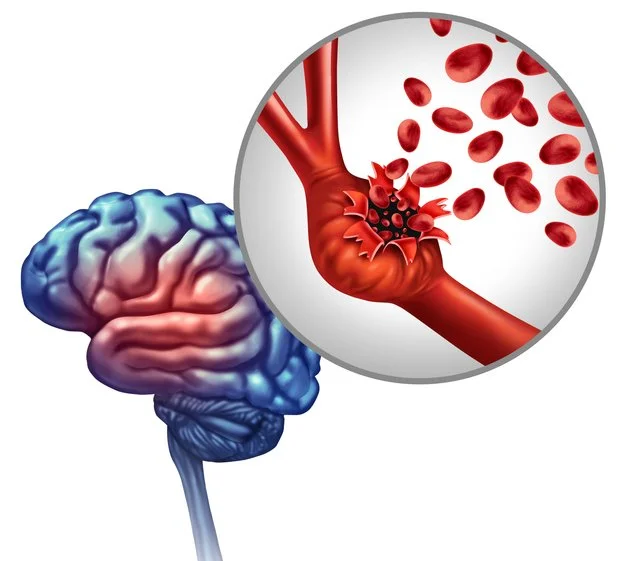
So, why might high-dose aspirin increase mortality? One reason is aspirin’s well-known side effects, especially its tendency to promote bleeding. Aspirin works by inhibiting thromboxane A2, a compound that induces platelet aggregation, which helps lower the risk of blood clots. However, this same mechanism can lead to gastrointestinal bleeding and intracranial hemorrhages—risks that may outweigh any cardiovascular benefits, particularly with long-term or high-dose use.
The Cancer Connection: Inconclusive but Intriguing
The role of aspirin in cancer prevention has been a topic of debate. Some studies suggest that long-term use of aspirin may lower the risk of certain cancers, such as colorectal cancer. However, this particular study found no significant association between aspirin use and reduced cancer mortality.
Low-dose aspirin showed a modest but statistically insignificant reduction in cancer deaths (hazard ratio: 0.80, 95% confidence interval: 0.60–1.08), while high-dose aspirin demonstrated no clear benefit (hazard ratio: 1.10, 95% confidence interval: 0.67–1.80).
Given these mixed results, further research is needed to fully understand aspirin's potential as a cancer prevention agent.
Age Matters: Aspirin’s Efficacy Declines with Time
One of the most notable findings of this study is how age affects the impact of aspirin. For participants aged 60 and older, high-dose aspirin was associated with an increased risk of cardiovascular disease (CVD) mortality. This finding aligns with recent guidelines from the U.S. Preventive Services Task Force, which no longer recommends routine aspirin use for primary prevention in adults over 60 due to the heightened risk of bleeding.
In contrast, younger adults (aged 40 to 59) who have elevated cardiovascular risk may still benefit from low-dose aspirin. However, this recommendation should be subject to individual risk assessments and a thorough consideration of bleeding risks.
Bleeding: The Double-Edged Sword of Aspirin Therapy
Aspirin’s ability to prevent blood clots presents a double-edged sword. While it reduces the risk of atherothrombosis, it also increases the likelihood of bleeding events. This is particularly concerning for older adults, whose tissues are often more fragile and less resilient to injury. Studies indicate that the risk of major gastrointestinal bleeding is nearly doubled among those who use aspirin, especially in older adults, who face the greatest dangers.
This delicate balance between the benefits and harms of aspirin underscores the importance of personalized medicine. Instead of using a one-size-fits-all approach, clinicians must carefully evaluate the individual risks and benefits of aspirin for each patient.
The Future of Aspirin in Preventive Medicine
So, what is the role of aspirin in preventive medicine? This study indicates that a more cautious approach is necessary. For individuals without a history of cardiovascular disease (CVD), the routine use of low-dose aspirin does not provide clear benefits and may expose them to unnecessary risks. On the other hand, high-dose aspirin seems to carry significant dangers, especially for older adults.
Future research should aim to identify specific subgroups that might benefit from aspirin therapy, such as individuals with genetic predispositions to clotting disorders or those with a history of recurrent cardiovascular events. Additionally, more studies are needed to examine the long-term effects of aspirin on cancer prevention and overall mortality.
Conclusion: Rethinking Aspirin’s Role
Due to emerging evidence, aspirin’s reputation as a wonder drug is being called into question. While it continues to be a valuable option for secondary prevention in individuals with established cardiovascular disease (CVD), its effectiveness for primary prevention is increasingly being scrutinized. This study emphasizes the need for personalized guidelines that consider factors such as age, dosage, and individual risk factors rather than applying blanket recommendations.
Ultimately, the decision to use aspirin should involve a discussion with a healthcare provider, balancing its potential benefits against the associated risks. As scientific knowledge evolves, our understanding of how to best utilize this common yet complex medication should also adapt.
Source:
Chen Y, Chen F, Liao J, Han H, Li G, Zhou L. Low- or high-dose preventive aspirin use and risk of death from all-cause, cardiovascular disease, and cancer: A nationally representative cohort study. Front Pharmacol. 2023 Feb 15;14:1099810. doi: 10.3389/fphar.2023.1099810. PMID: 36874020; PMCID: PMC9974638.