Stop the Cholesterol Madness
This post is not intended to diagnose or treat any illness.
After repeated conversations with me, a close relative in his late 50s decided to try the carnivore diet. He immediately began to feel better than he had ever felt. The carnivore diet is ultra-low-carb, similar to the ketogenic diet, which often raises LDL and total cholesterol. He has lost 22 pounds, lowered his BMI from 25.8 (overweight) to 22.8 (normal), lowered his blood pressure from 110/70 to 100/66, has more energy, lowered his triglycerides from 106 to 71 (lower is better), raised his HDL from 47 to 79 (higher is better), lowered his VLDL by 1/3, rid himself of chronic foot and hip pain, and he has no more leg cramping. As we will see later in this post, these changes indicate inflammatory, metabolic, and cardiovascular health improvements.
At the same time, he raised his LDL from 69 to 192 and his total cholesterol from 137 to 285, which made his doctors panic. Later in this post, we will see that LDL levels below 105 cause twice the amount of death. Despite this, his doctors have ignored nine positive changes and stressed two that, as we will see in this post, have little relevance in their ability to predict cardiovascular disease. What kind of a world do we live in when doctors fret when their patients become healthier? Read on if you are curious.
Uffe Ravnskov
According to Uffe Ravnskov in his 2018 paper called LDL-C does not cause cardiovascular disease: a comprehensive review of the current literature, which is the basis of the information presented in this post, the idea that high cholesterol levels in the blood are the main cause of heart disease (Cardiovascular disease, CVD) is impossible. People with low levels become just as atherosclerotic (get heart disease) as those with high levels, and their risk of heart disease is the same or higher. The cholesterol hypothesis has been kept alive for decades by reviewers using misleading statistics, excluding the results from unsuccessful trials, and ignoring numerous contradictory observations. Furthermore, the cholesterol hypothesis fails to satisfy the Bradford Hill criteria for causality, which is the standard to assess causation.
In short, according to Dr. DuBroff and de Lorgeril, the diet-heart hypothesis survives only because its proponents selectively cite evidence that validates their own viewpoint while disregarding evidence to the contrary. Consequently, the field of cardiovascular care is built upon dubious information.
Upton Sinclair
The quote by Upton Sinclair, It is difficult to get a man to understand something when his salary depends upon his not understanding it, explains what is happening in the coronary care/blood lipid field. As we will see later in this post, other markers give a much more accurate picture of cardiovascular fitness, none of which have medications to alter them. However, changing them requires only lifestyle modifications of diet, exercise, and sleep, which are not money-makers for doctors. I recommend a visit to Dr. Davis at drdavisinfinithealth.com for a fresh view of a cardiologist who gets it. In his own words, He "was in the business of dispensing prescription drugs and procedures, not health. Once he rejected conventional notions of delivering "health" through drugs and procedures and instead began to seek out ways to restore health naturally, logically, inexpensively, so many answers became apparent. Delivering these ideas to people has resulted in reversing hundreds of common health conditions, effortless weight loss, day-to-day functioning at higher levels, as well as many age-reversing effects."
Familial Hypercholesterolemia
If high total cholesterol causes atherosclerosis (heart disease), people with high total cholesterol should have more atherosclerosis than people with low total cholesterol. In 1936, Landé and Sperry found that corrected for age, unselected people with low total cholesterol were just as atherosclerotic as people with high total cholesterol. Since then, their seminal observation has been confirmed in at least a dozen studies. A weak association between total cholesterol and the degree of atherosclerosis has been found in some studies, but the authors only studied patients admitted to a hospital and may, therefore, have included patients with familial hypercholesterolemia (FH).
A subset of FH patients with CVD susceptibility may develop heart disease regardless of their LDL levels. For instance, Jansen et al. found that patients with a polymorphism for the prothrombin gene had a higher incidence of CVD than those without the polymorphism despite having similar LDL levels. So, there may have been a bias introduced as cardiology departments have a higher percentage of patients with atherosclerosis. When patients with total cholesterol levels above 350 mg/l were excluded, representing the subjects with FH, the positive association between total cholesterol and degree of atherosclerosis (heart disease) in the study by Solberg et al. disappeared. Incidentally, elderly individuals with familial hypercholesterolemia (FH) have the same risk of cardiovascular disease (CVD) mortality as those without FH despite lifetime exposure to high LDL. This finding contradicts the hypothesis that LDL causes atherosclerosis and that CVD risk increases with the duration of LDL exposure. 1
High Cholesterol and Statins
If high total cholesterol (TC) were the main cause of atherosclerosis, there would be a correlation between cholesterol-lowering drugs and reduced risk; however, in a review of 16 cholesterol-lowering trials, such a correlation was found in only one that correlated lower total cholesterol to less heart disease, where the treatment was exercise!
If high LDL were the main cause of CVD, statin treatment would be more effective with greater LDL reduction. However, the response was absent in all three clinical trials that calculated it. According to Kristensen et al., statin treatment does not prolong lifespan by more than an average of a few days. Lastly, since 2005, health authorities in Europe and the United States have required all trial data to be made public. As a result, claims of benefit from statin trials have virtually disappeared.
Total Cholesterol Lies
If high total cholesterol causes heart disease, people with it would have a higher risk of dying from it. The hypothesis was introduced in the 1960s by the authors of the Framingham Heart Study. In their 1987 study, the authors found that a 1 mg/dl drop in total cholesterol per year resulted in an 11% increase in coronary and total mortality over 30 years! Sadly, the American Heart Association and the U.S. National Heart, Lung, and Blood Institute cited the Framingham study and falsely announced that a one percent drop in cholesterol reduces cardiovascular risk by 2%, a blatant deception.
In two more reviews by supporters of the cholesterol hypothesis, the researchers searched for quotations from 12 relevant articles in the three reviews. Only two articles were quoted correctly, while about half of the contradictory ones were ignored. Additionally, statistically nonsignificant findings favoring the cholesterol hypothesis were inflated, and unsupportive results were quoted as supportive in the remaining articles. Only one of the six randomized trials aimed at reducing cholesterol levels that reported negative results was cited, and this was only mentioned in one of the reviews.
LDL
If high LDL caused heart disease (CVD), untreated patients with CVD would have higher LDL levels than normal. However, a large American study found that almost 140,000 patients with acute myocardial infarction had lower LDL levels than normal upon admission to the hospital. In a study with similar findings, patients with LDL below 105 mg/dl had twice the total mortality rate compared to those with higher LDL, even after adjusting for confounding variables, at a follow-up three years later.
Inverse causation suggests that the inverse relationship between mortality and LDL might be because heart disease is linked to infections, and LDL directly deactivates almost all microorganisms and their toxic products. Healthy individuals with low LDL are more likely to get infectious diseases and cancer, potentially because microorganisms are responsible for nearly 20% of all cancer types.
If high LDL were the primary cause of atherosclerosis and CVD, individuals with high levels should have shorter lives than those with low values. However, a recent systematic review of 19 cohort studies, which included more than 68,000 older adults (>60 years of age), found people with high LDL lived longer.
Finally, elderly individuals with high LDL levels for decades do not have higher CVD mortality or morbidity, including ischemic stroke, than the general population, which challenges the lipid hypothesis that high LDL is inherently atherogenic.
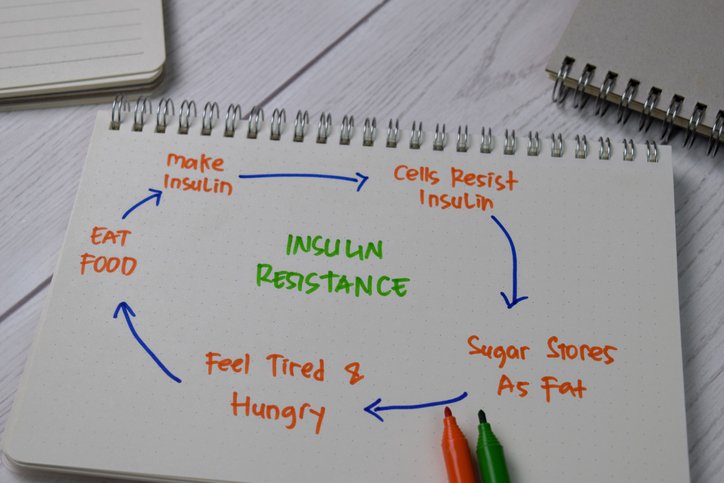
Insulin Resistance
A lot of research shows that there are other things to look at besides your cholesterol when figuring out your risk of heart disease. One of the biggest things to pay attention to is insulin resistance, which happens when your body has trouble using insulin properly, and it can lead to type 2 diabetes, a really big risk factor for heart disease. So yeah, it's not just about LDL cholesterol!
Small, Dense LDL Particles
It's not just your LDL or total cholesterol levels determining your risk of atherogenic dyslipidemia. The size and density of your LDL particles have a bigger impact. Suppose you've got small, dense LDL particles. In that case, they can easily undergo atherogenic changes in your bloodstream, which can increase your cardiovascular risk, and this goes for anyone, especially those with familial hypercholesterolemia.
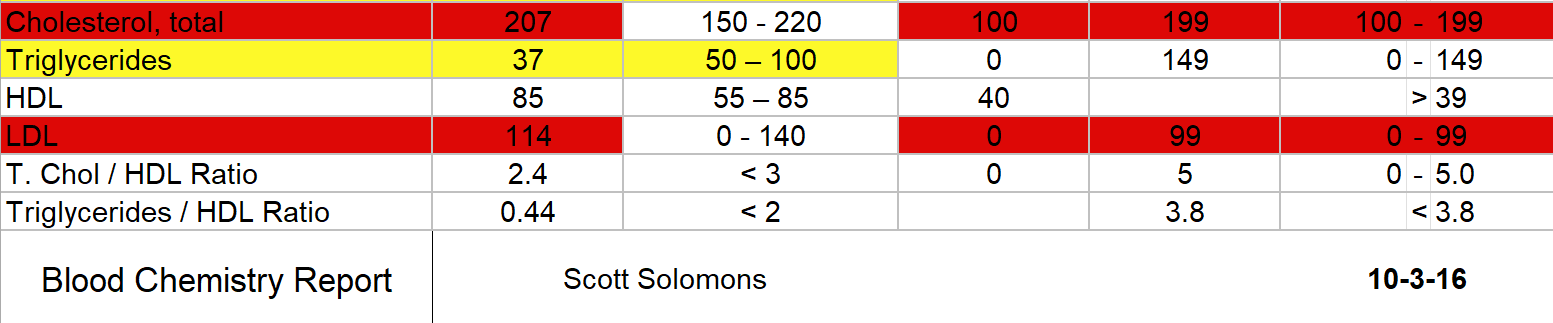
Triglyseride:HDL Ratio
Having high levels of triglycerides (TGs) and low levels of HDL (the "good" cholesterol) can increase your risk of heart disease. Even if your LDL (the "bad" cholesterol) levels are low, having a high ratio of TGs to HDL can still predict an increased risk of cardiovascular issues. According to a study by Caselli and colleagues, this risk is independent of any lipid-lowering treatments you may be taking. So, it's important to monitor your TGs/HDL levels and not just focus on your LDL. Incidentally, a high triglyceride to HDL ratio is a proxy for small, dense LDL particles. The test above is mine from a few years back. First, my total cholesterol and LDL are high, which I love. Second, my HDL(the good one) is so high, it is marked as an outlier in yellow. Finally, my triglyceride to HDL is only .44. Anything below two is considered ideal. This test would scare the average doctor and cause them to automatically prescribe a statin. No thanks.
Low Carb and Carnivore Diets Effect on Cholesterol
Low-carb diets like the carnivore diet are really good for reducing the risk of atherogenic dyslipidemia triad. Plus, they can help you lose weight and improve your HDL levels while decreasing triglycerides and C-reactive protein, a marker for inflammation. Cole and colleagues investigated the impact of increased fat and cholesterol intake within a low-carb diet, resulting in decreased triglycerides and increased HDL levels without affecting LDL-C levels.
Another study compared low-carb diets to low-fat diets in some obese adults; the low-carb diet was the clear winner. Another meta-analysis showed that low-carb diets can reduce the risk of atherosclerotic cardiovascular disease by lowering plasma triglycerides and raising HDL levels. In summation, dietary change can improve (lower) your triglyceride to HDL ratio.
Are Low-Carb Diets Safe Long-Term?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8594484/
Longer-term trials and individual case reports demonstrate the effectiveness and sustainability of these diets. After one year, participants with type 2 diabetes who followed a ketogenic diet showed significant improvements in multiple cardiovascular risk factors. These included lowered levels of triglycerides, small dense LDL particles, blood pressure, and antihypertensive medication use. The safety and effectiveness of the ketogenic diet in treating epilepsy were documented by Heussinger et al. over ten years without evidence of increased CVD risk biomarkers from low-carb diet effects. Rather than weight or fat loss, carbohydrate restriction primarily improves cholesterol and triglycerides (atherogenic dyslipidemia). 2
Low Carb Studies and CVD
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(94)90566-5/fulltext
So, two studies examined whether people with high LDL (the "bad" cholesterol) and high HDL and low triglycerides are more likely to have heart problems. The first study called the 4S trial, had researchers looking at whether taking statins could help prevent heart problems in people who had high levels of LDL cholesterol and either a 1) high level of triglycerides and a low level of HDL cholesterol (which are bad for your heart) or a 2) low level of triglycerides and high level of HDL cholesterol (which are good for your heart). They compared the results to those who didn't take anything. The people with high HDL and low triglycerides had fewer heart issues than those in the low HDL high triglyceride group, even though both had high LDL.
The second finding in the 4S reanalysis examined how statin treatment affects coronary events. They found it only works for people with high triglycerides and low HDL ratios. If you have a more low-carb-diet-like profile, statins won't do much for you. Even if your LDL levels drop the same amount as someone with an atherogenic profile, you won't see a reduction in hard coronary events. If you've got high LDL, low triglycerides, and high HDL, statins may not be the right treatment.
The second study, the PROSPER study, found that statin treatment only benefited subjects with low HDL, regardless of their LDL levels.
Conclusion
Dr. DuBroff and de Lorgeril state that "the diet-heart hypothesis survives only because its proponents selectively cite evidence that validates their own viewpoint while disregarding evidence to the contrary." The industry rests on a fragile foundation and must ignore potential solutions to maintain profits. Significant metabolic changes from lifestyle and dietary modifications could significantly reduce cardiovascular disease, but this would require a complete restructuring of cardiology. To requote Sinclair, It is difficult to get a man to understand something when his salary depends upon his not understanding it.
Source:
Uffe Ravnskov, Michel de Lorgeril, David M Diamond, Rokuro Hama, Tomohito Hamazaki, Björn Hammarskjöld, Niamh Hynes, Malcolm Kendrick, Peter H Langsjoen, Luca Mascitelli, Kilmer S McCully, Harumi Okuyama, Paul J Rosch, Tore Schersten, Sherif Sultan & Ralf Sundberg (2018) LDL-C does not cause cardiovascular disease: a comprehensive review of the current literature, Expert Review of Clinical Pharmacology, 11:10, 959-970, DOI: 10.1080/17512433.2018.1519391