Unintentional Oxalate Overload on a "Healthy Diet"
Disclaimer: The content provided in this post is for informational purposes only and should not be construed as medical advice. It is not intended to replace professional medical diagnosis, treatment, or guidance. Always consult with a qualified healthcare provider before making any changes to your diet, exercise regimen, or medical treatment plan. The author and publisher of this blog post are not liable for any potential health consequences resulting from the use of the information provided.
You may have heard of oxalate because it is infamously implicated in kidney stone formation. Oxalate is damaging in higher concentrations, cannot be metabolized, and needs to be excreted. Given their direct role in oxalate excretion, the kidneys often sustain the most severe damage in states of oxalate excess, but other tissues can suffer as well. This post will cover oxalate, what foods contain it, the problems it can cause, and what to do about reducing oxalate if you are experiencing a problem.
The Oxalate Compound
Oxalate has a negative charge and a chemical formula of C2O4 and contains two carbons and four oxygen atoms. Because of this, it is classified as an anion. It has a charge of negative two, so technically, it is a dianion. It is found in many plants, and the human body produces it in smaller amounts.
Foods (only vegetables) Containing Oxalate
Rhubarb, buckwheat, star fruit, black pepper, parsley, poppy seeds, amaranth, chard, beets, cocoa, nuts, berries, spinach, soy, potato, legumes and beans, avocado, citrus, and dates. A major source is from seed oils like soybean oil. I will include a special section for oxalte from seed oils.
Normal Absorption of Oxalate
Normal intestinal absorption of oxalate is around 10–15%, but it varies depending on diet. For instance, because oxalate bound to calcium is not absorbed, low-calcium diets have been linked to increased oxalate absorption. Similarly, in individuals with small bowel malabsorption syndrome, oxalate uptake is increased because of a reduction in free intestinal ionized calcium. In addition, gut microbiome dysbiosis might affect intestinal oxalate availability and, thus, its urinary excretion. 2
How We Handle Oxalate After Absorption
The human body produces 12mg of oxalate every day. The kidneys filter and concentrate oxalate more than other organs in the body. It is unknown how much oxalate other tissues in the body can handle, but studies suggest that we can safely handle 50mg/day excreted by the kidneys. To achieve 50mg/day of kidney excretion, one would need to consume 500mg/day of oxalate. Typically, 25mg of oxalate is excreted by the kidneys each day, which means that a daily limit of 250mg of oxalate should be observed. 3
Abnormal Oxalate Absorption
Normally, calcium binds to oxalate, preventing it from being absorbed. Conditions such as gastrointestinal surgeries, inflammatory bowel diseases, and malabsorption syndromes bind calcium away from the oxalate, causing increased absorption of oxalate. Additionally, consuming foods high in oxalate or precursors can result in substantial oxalate absorption. Oxalate cannot be metabolized, and it must be excreted in urine, regardless of its source. When the level of calcium oxalate supersaturation exceeds the point of spontaneous crystallization, oxalosis may occur as calcium oxalate begins depositing throughout the body, causing pain, inflammation, and kidney stones. 4 Oxalosis has been described as far back as 1844 when it was referred to as oxalic acid diathesis. 5
Oxalate From Seed Oil Ingestion
Seed oils include soybean, canola, corn, sunflower, safflower, and others. A major source of oxalate is glyoxalate, which is converted from glyoxal, which is found in high amounts in seed oils. Oxalate is a mitochondrial toxin, diminishing the production of energy through the citric acid cycle by 48%. The result is low energy. Chris Masterjohn has some excellent information on the subject. 6
Health Problems Associated With Excess Oxalate
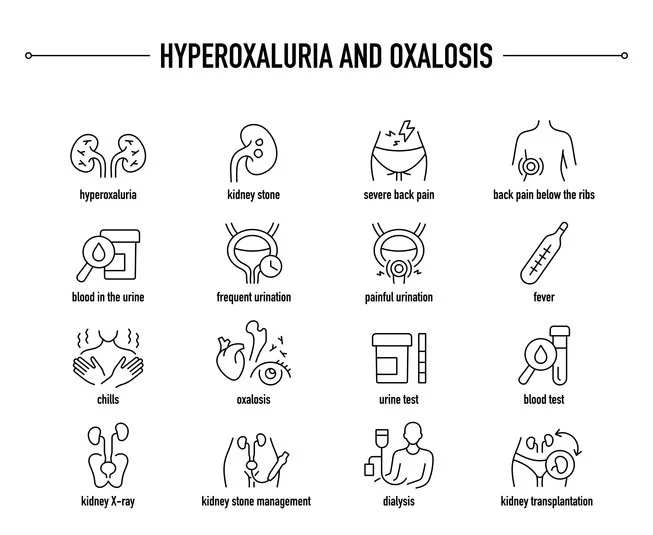
Hyperoxaluria: Oxalate is easily measured in the urine. A high level of oxalate in the urine is called hyperoxaluria. Although only sometimes problematic, it may indicate there is a medical problem. Certain intestinal issues can cause the body to absorb excessive amounts of oxalate from food, leading to an increase in the concentration of oxalate in urine. Crohn's disease is one such condition that can result in enteric hyperoxaluria. Another condition that can cause this problem is short bowel syndrome, which may occur after the surgical removal of certain parts of the small intestine. When a person's small intestine faces difficulty in absorbing fats from food, they may experience problems with oxalate absorption as well. As I have mentioned, oxalate usually binds with calcium in the gut and is eliminated from the body through stools. However, when there is an excess of fat in the gut, calcium attaches to the fat, making oxalate available for absorption in the bloodstream. This can lead to increased levels of oxalate in the kidneys. Additionally, Roux-en-Y gastric bypass surgery can also result in reduced absorption of fats in the gut, which increases the risk of hyperoxaluria.
Kidney Stones: An increased load of dietary oxalate presented to the kidneys has been linked to different kidney-related conditions and injuries, called nephritis or nephropathy. The most studied consequence of increased urinary oxalate excretion is calcium oxalate nephrolithiasis, otherwise known as kidney stones.
Arthritis: Oxalate arthritis can occur when calcium oxalate crystals build up in bones, tendons, cartilage, and synovium. These crystals may move into the synovial fluid, leading to an inflammation response that causes joint pains, also called arthralgias. The fingers, toes, spine, and shoulders can be involved.
Heart Problems: Patients with cardiac involvement may present with arrhythmias due to crystal deposition within the conduction system. They may also present with palpitations, syncope (fainting), dyspnea (labored breathing), and rarely chest pain. Cardiac imaging may reveal valvular abnormalities and evidence of an infiltrative process with impaired right and left cardiac output.
Gout: The highly insoluble iron oxalate appears to play a major role in gout, the nucleation and growth of the otherwise extremely soluble sodium urate. This explains why gout usually appears after age 40, when ferritin, the storage molecule of iron, levels in blood exceed 1 μg/L 7
High Oxalate Diets Today
The foods I listed at the beginning of this post are considered part of a nutritious diet, which presents the increasing possibility of medical conditions specifically related to the consumption of extremely high levels of certain nutrients. The practice of juicing is widespread, and almond milk is very common. Shelled nuts can be eaten by the handful. Additionally, agricultural products are available in all seasons, making it possible to burden the body with overdoses of nutrients like beta carotene, oxalates, saponins, xenoestrogens, and more.
BMJ Case Study
In one case described in the British Medical Journal, a patient consumed many different foods with high oxalate levels, although all in moderation of 1–2 servings per day. Even by practicing the belief of 'everything in moderation' (I don't believe in moderation; optimization is my thing), the patient still consumed nearly 1500 mg of oxalate daily, up to 10× greater than the average American. To put things into perspective, one cup of cooked spinach contains about 1510 mg of oxalate. Overdosing is easy.
He was consuming over a liter of almond milk every day, along with wheat germ and a variety of other nuts. After his first visit to a kidney clinic, he became increasingly concerned about his prostate health and decided to increase his intake of antioxidants. He started consuming more foods that he believed would benefit his health, including 2-3 tablespoons of tomato paste per day, a handful of Brazil nuts, hazelnuts, walnuts, pistachios, pecans, almonds, several teaspoons of cocoa powder and wheat germ, and 500 mg of vitamin C daily. He also continued to drink at least a liter of almond milk each day. Unfortunately, he was unaware of the potential risks associated with excess oxalate in these foods. He developed several days of nausea, vomiting, anorexia, and lethargy and was admitted to the hospital. A history of consuming oxalate precursors was discovered upon further dietary investigation. A kidney biopsy confirmed oxalate nephropathy. The patient's recovery was achieved by limiting oxalate consumption, increasing hydration, and administering oral calcium acetate. 8
My Experience
As some of you know, I am in the fourth year of eating an animal-based diet with almost no vegetable intake, so I have zero oxalate intake. I experienced a sudden remission of lateral epicondylitis, which is a pain in the elbow tendon, and an eight-month disappearance of tenosynovitis, which is a pain in the finger joints in my thumb. I can't be 100% sure, but eliminating the oxalate was probably the reason for my cure. Incidentally, I have never had any kidney stones, and my gut is healthy; for these reasons, I believe I have a normal ability to clear oxalate. I am not suggesting that you need to go on an animal-based diet or eliminate oxalate from your diet. However, if you have any unexplained pain, oxalates should be considered as a contributor. I have written about plants' chemical defense mechanisms before. Too much of the wrong one can lead to health problems. I am not suggesting abandoning eating vegetables and fruit, but they are not the miracle foods some claim they are. I strongly recommend avoiding seed oils at all costs.
Conversely, animal-based foods are better for you than many would have you believe. They are associated with a longer lifespan. Read this post for more on the subject. Chronic problems like joint pain have been cured by switching to the carnivore diet, but most people choose not to go that route. Therefore, should you find yourself with mysterious medical problems, consider oxalate as a contributing factor.